What is Denial Management in Medical Billing? A Comprehensive Guide for Healthcare Providers
Denial Management in Medical Billing is a crucial process that healthcare providers need to use to deal with refused claims efficaciously. This guide is comprehensive and will cover the most important elements that make up denial administration, different kinds methods for managing denials and perfect strategies for healthcare providers.
Definition and Importance of Denial Management
The term Denial Management in medical billing is the systematic method of the identification, analysis and resolving claims that are denied from insurance companies and other payers. This is essential due to:
- The denial of claims can have a significant impact on the revenue stream of a healthcare company which could lead to financial loss.
- Effective denial management increases efficiency of operations and boosts overall performance of the revenue cycle.
- In reducing the number of claims denied, healthcare organizations can increase cash flow and ease administrative charges.
Types of Denial Management Strategies
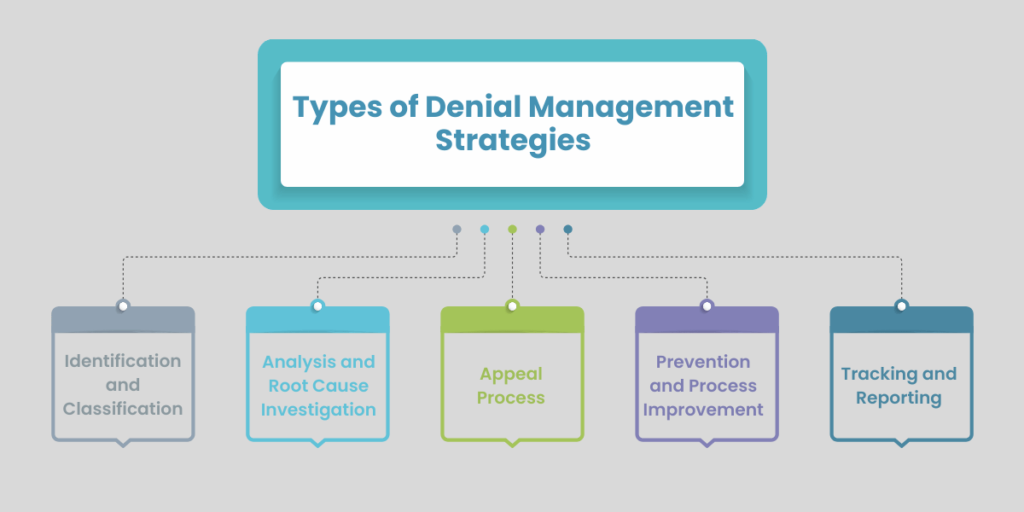
Healthcare professionals can use a variety of strategies to deal with rejected claims definitely. Here are a few of the most commonly used strategies:
1. Identification and Classification:
This requires the systematic identification of denied claims and classifying them compatible to the reasons behind their the denial. A proper classification allows the analysis and resolution of particular problems.
2. Analysis and Root Cause Investigation:
A thorough review of denied claims will help determine the root causes behind denied claims. This might involve review of the patient’s information, coding accuracy and completeness of documentation, or eligibility issues.
3. Appeal Process:
When the reason behind denial is established The following step will be to challenge the denial. This requires extensive document and submission on time within the payer-specific deadlines.
4. Prevention and Process Improvement:
Based on the insights gained through denial analysis Based on the findings from denial analysis, healthcare providers can put in place strategies to avoid similar denials in the near future. This could include education for staff and training, enhanced data collection methods, improved codes practices, or modifications to policies.
5. Tracking and Reporting:
Monitoring claims that are denied in time allows healthcare providers to keep track of trends, assess how effective their interventions are and constantly rise their strategies for managing denials.
Key Components of Effective Denial Management
In order to implement a reliable approach to managing denied requests, medical professionals must focus on these important elements:
- The timely identification and classification of claims that are denied
- An in-depth analysis of the denial motives
- A speedy appeal process backed by extensive documentation
- Continuous process improvement Based on the denial patterns
- Regularly tracked and reported on the rates of denial and resolutions
Optimal Practices for Healthcare Providers
Implementing these accurate techniques can dramatically improve the denial management capabilities of a healthcare provider. capabilities:
- Consider investing in software for managing denials to simplify the process and make it easier to track.
- Regularly train your employees on proper coding, documentation and billing procedures.
- Create a quality assurance program to spot mistakes before the process of billing.
- Keep open channels of communication with the payers to clarify the requirements and resolve any issues quickly.
- Think about outsourcing the management of denials to specialist service providers If resources are not sufficient.
Conclusion
Denial Management of medical bills is a challenging but essential process for healthcare professionals. Implementing effective strategies and investing in software for denial management and adhering to excellent guidelines, healthcare facilities can dramatically reduce the number of claims denied, boost revenue cycle performance and increase overall efficiency.
Be aware that, although the typical rate of claim denial can vary from 5% to 10%, the majority of denied claims are avoidable and as high as two-thirds of denied claims could be recovered. If you focus on proactive denial management healthcare professionals can improve their financial performance and provide superior healthcare to patients.
Frequently Asked Questions?(FAQ's)
Denial management refers to identifying, analyzing, and resolving denied claims from insurance companies or payers. It's crucial because denied claims directly impact a medical practice's revenue stream.
Denials are a direct block to revenue. They delay incoming payments, consume labor hours, and in the worst-case scenario, result in uncompensated care. Proactive denial management helps maintain a sustainable financial position.
Denial management in medical billing offers several key benefits, including improved cash flow and revenue through reduced claim denials, enhanced operational efficiency by streamlining processes, and better patient care satisfaction by addressing billing issues promptly.
Denial management in medical billing typically involves identification and classification, analysis and root cause investigation, and appeal processes. Other key types include prevention and process improvement, tracking and reporting, and automation using advanced billing software. These strategies work together to optimize cash flow, enhance operational efficiency, and improve overall revenue cycle performance in healthcare organizations.
Practices can implement strategies such as:
- Accurate patient registration and thorough documentation
- Regular staff training on coding and billing guidelines
- Timely submission of claims
- Conducting regular audits to identify and address potential issues before claims are submitted.