- Mon - Sat: 8.00 - 18.00
- The Green STE A DOVER DE 19901
- +1 (302) 231-1207
revenue cycle management
Streamline Your Revenue Cycle with Collectronix
Let us handle the financial side of your practice so you can focus on providing quality patient care. Our expert services enable you to streamline financial processes, minimize errors, and ultimately enhance your organization’s profitability.
What is Revenue Cycle Management?
Revenue Cycle Management (RCM) is a multifaceted process within the healthcare sector that entails overseeing all financial transactions and engagements between a healthcare institution and its patients throughout the entire continuum of care. This encompasses the complete lifespan of a patient’s account, commencing from their initial point of contact and appointment scheduling and culminating with the settlement of the outstanding balance.
In the ever-evolving healthcare environment, the significance of RCM cannot be overstated. In this intricate and dynamic field, proficient RCM practices are paramount to ensuring the financial stability and endurance of healthcare organizations, spanning a spectrum that includes forward-thinking primary care facilities and independent medical practices.
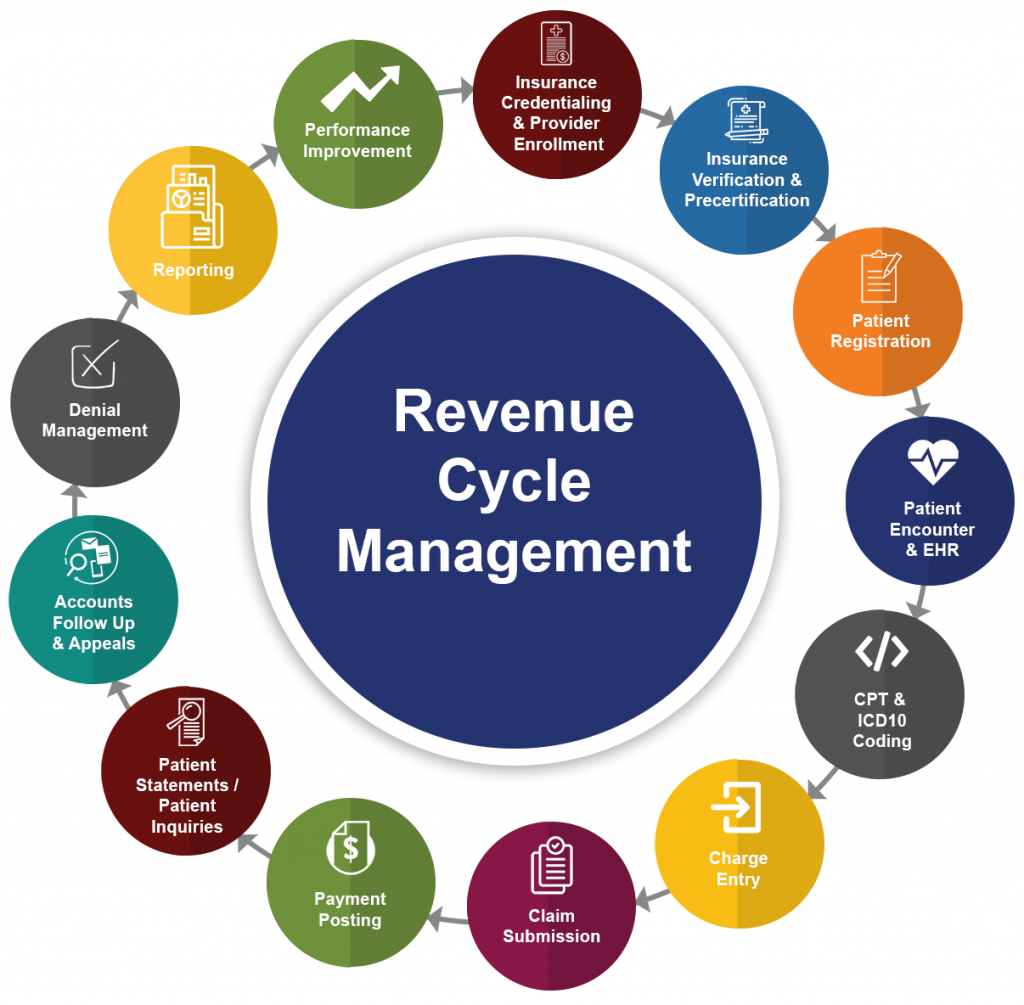
Understanding the Revenue Cycle Management Process
The Revenue Cycle Management (RCM) process is a sequence of essential steps that healthcare organizations adhere to in order to proficiently oversee the financial aspects of patient care. Let’s delve into the key stages:
Patient Registration
The RCM process commences with patient registration, during which vital demographic and insurance information is gathered. This step is pivotal for establishing precise patient records and ascertaining insurance coverage. Additionally, pre-authorization may be required for specific procedures to ensure that the services are approved by the payer.
Coding & Charge Capture
Following the provision of care to the patient, medical coders assign alphanumeric codes to document the diagnoses, procedures, and services rendered. These codes play a critical role in billing and reimbursement. Charge capture encompasses the meticulous recording of all billable services and procedures to guarantee accurate billing for the care provided.
Claims Submission
In this stage, the coded information is utilized to generate and submit claims to insurance payers. This entails the preparation and submission of electronic or paper claims containing pertinent patient and service details. Subsequently, payers evaluate and process of these claims, determining the reimbursement amount for the services rendered.
Accounts Receivable
Accounts Receivable (AR) management involves the diligent monitoring and administration of payments from both patients and insurance companies. This encompasses tracking outstanding balances, pursuing unpaid claims, and ensuring the timely collection of payments. Effective AR management is of utmost importance in financial stability.
Optimize Your Revenue Cycles with Collectronix's Expert Solutions
Discover how Collectronix can help you maximize revenue efficiency through our comprehensive revenue cycle management solutions. Our expert services enable you to streamline financial processes, minimize errors, and ultimately enhance your organization’s profitability.
Advantages of Healthcare Revenue Cycle Management
The advantages of proficient Healthcare Revenue Cycle Management extend broadly, influencing the financial stability of healthcare institutions and the quality of patient care. Let’s explore the specific benefits:
Improved Payer Negotiations: Effective RCM empowers healthcare organizations in payer negotiations. A comprehensive grasp of financial data and performance metrics enables providers to secure more favorable contracts with payers. This includes negotiating better reimbursement rates and terms that align with the organization’s financial objectives.
Timely & Accurate Reimbursement: A well-coordinated RCM process guarantees the accurate and punctual submission of claims. Consequently, the reimbursement process accelerates. Timely submissions reduce the risk of claim denials and ensure healthcare providers receive payments promptly, fostering consistent cash flow.
Reduced Bad Debt: Proficient RCM practices help identify and address potential issues with patient payments at an early stage. This involves verifying insurance coverage, providing transparent communication regarding patient financial responsibilities, and implementing efficient billing procedures. Consequently, the risk of bad debt—unpaid or irrecoverable patient balances—is significantly diminished.
Increased First-Submission Claim Success: A robust RCM process targets a high rate of claims being paid after the initial submission. This reduces the need for time-consuming and resource-intensive appeals. Accurate first-time claim submissions enable healthcare organizations to streamline their operations, minimize reimbursement delays, and enhance overall efficiency.

The Role of Electronic Health Records (EHRs) in RCM
Electronic Health Records (EHRs) play a pivotal role in streamlining Revenue Cycle Management (RCM) processes. They revolutionize how documentation and coding are handled in the following ways:
Real-Time Access
EHRs offer instant access to comprehensive patient data, empowering healthcare providers and administrators with up-to-the-minute information for quicker and more accurate decision-making. This ensures billing processes are well-informed.
Streamlined Claims
EHRs simplify the claims submission process, allowing billing staff to create claims directly from digital records, reducing the likelihood of manual data entry errors. Electronic claims submission expedites payer processing.
Automated Alerts
EHRs automate billing and coding reminders, enhancing regulatory compliance, reducing denials, and optimizing the revenue cycle. Automated alerts flag missing information or coding discrepancies before claim submission.
Enhanced Collaboration
EHRs promote improved communication and collaboration among RCM departments. A centralized platform ensures seamless information sharing between front-end staff and billing teams, reducing communication gaps.
Data-Driven Insights
EHRs include data analytics capabilities that offer valuable insights into healthcare organizations' financial performance. By analyzing key metrics, organizations can pinpoint areas for improvement, streamline workflows.
Efficient Documentation
Electronic Health Records (EHRs) simplify data capture, enhancing accuracy. This digital transition eliminates paperwork, streamlining the coding process. Detailed EHR documentation aids coders, reducing errors.
