- Mon - Sat: 8.00 - 18.00
- The Green STE A DOVER DE 19901
- +1 (302) 231-1207
denial management
Elevate Your Financial Success by Implementing Our Comprehensive Denial Management Solutions
Our Specialists Employ a Streamlined Approach to Monitor Every Claim, Ensuring Efficient Aging AR Recovery
Revolutionizing Of Denial Management
1-Denial Reason Categorization
We systematically categorize the identified reasons and delegate them to the relevant teams, ensuring prompt and effective corrective measures.
2-Filing New Claims
After the receipt of claims from various departments, a subsequent step involves resubmitting them for processing.
3-Identifying Denial Root Causes
We employ a detailed investigative process to thoroughly understand and address the underlying causes of claim denials.
4-Tracking Future Claims
Implementing a Secondary Review System Rooted in Analysis of Denial Reasons to Proactively Mitigate Future Rejections and Enhance Claim Success Rates.
5-Creating a Prevention System
Strategically Constructing a User-Friendly Checklist to Systematically Identify and Resolve Common Denial Reasons, Streamlining the Claim Management.
6-Implementing a Tracking System
Ensuring Comprehensive Oversight and Continuously Monitoring the Progress of Resubmitted Claims with Regular Follow-ups for Efficient Processing.
Improving Clean-Claims Ratios via Denial Management Solutions.
Our Denial Management Services are designed to assist healthcare providers in identifying and rectifying the root causes of claim denials. This, in turn, leads to improved clean-claims rates, more efficient workflows, and faster appeals processes.
We provide customized recommendations to enhance documentation, claims management, and processes, all while proactively addressing regulatory compliance. Our interdisciplinary team, consisting of clinical, technical, and revenue cycle specialists, seamlessly integrates with various billing systems and EHRs. This integrated approach effectively resolves underpayments and alleviates the administrative burden associated with managing denied claims.
.

Transforming Denial Management through Revolutionary Practices at Collectronix
At Collectronix, we are at the forefront of a groundbreaking approach to denial management. Our commitment to innovation and efficiency has led us to revolutionize the way denials are handled.
Identifying the Reasons for Denials
Our Medical Billing Services utilizes a systematic approach to uncover the causes of claim denials. We meticulously investigate each denied claim, scrutinizing factors such as coding disparities, deficient patient information, and inconsistencies in service documentation
Classifying Denied
Claims
Once we identify denied claims, our subsequent action is to categorize them according to the specific reason for denial. Our categorization system includes a wide range of categories, such as missing information, coding mistakes, and services not covered by insurance.
Enhancing Claim
Resubmission
Upon identifying the reason for the denial, our team takes swift action to rectify the issue and initiate the claim resubmission process. This may involve correcting billing inaccuracies or providing the
missing information that led to the initial denial.
Tracking System
We understand the importance of closely monitoring the progress of each resubmitted claim. Our dedicated team keeps a watchful eye on the entire journey of each claim, meticulously tracking it from the point of resubmission to its final acceptance and payment by the payer.
Proactive Denial
Prevention
In addition to effectively resolving denied claims, our company has strategically implemented a proactive mechanism aimed at not only rectifying past denials but also at minimizing the likelihood of encountering future denials.
Ongoing Future Claims Monitoring
Last but not least, we maintain continuous oversight of future claims to guarantee their accuracy and completeness before submission. Our team collaborates closely with our clients to keep them informed about any potential issues or errors.
Strategies for Reducing Denials and Optimizing Revenue
in Medical Billing
Medical billing is a complex process, encompassing various stages from claim submission to payment receipt. However, one of the most significant challenges faced by medical billing companies is managing denied claims. Denials can occur for a variety of reasons, including coding errors, missing information, or services not covered, and they can have a significant impact on a healthcare provider’s revenue.
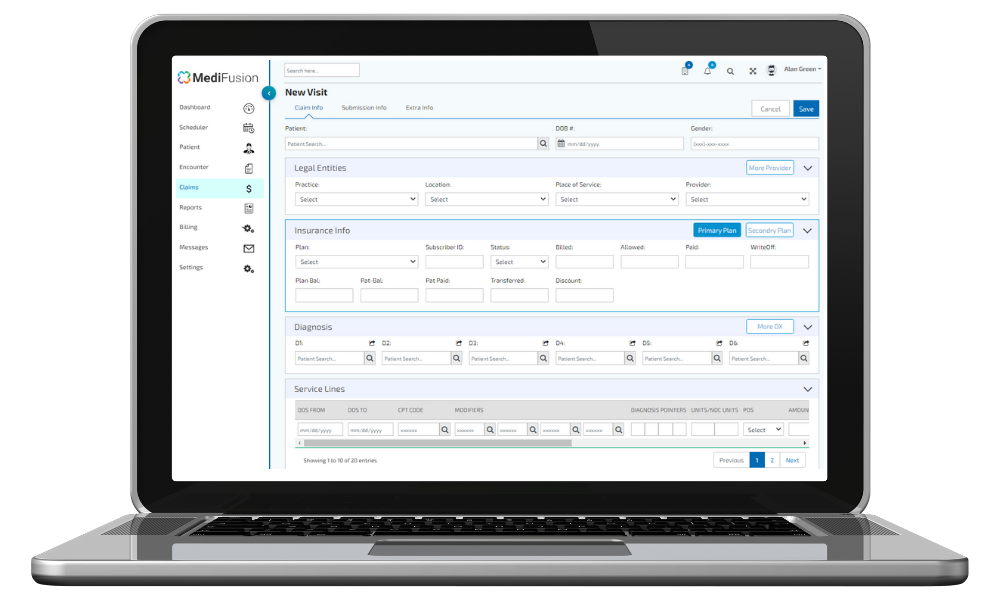
Improved Collection Rates
Our Denial Management team is dedicated to enhancing your payment recovery efforts. By identifying the underlying reasons for denied claims and equipping you with the essential resources for prompt resolution, we ensure an efficient process. Utilizing our integrated software suite, MediFusion, denied claims are automatically directed to the relevant team members, enabling swift follow-up and systematic corrections.
Rule-Based Denial Prevention
Our advanced claim scrubbing tool goes beyond mere error detection; it systematically identifies and corrects issues in claims before submission. Our fully adaptable rule-based system is tailored to prevent denials associated with coding, LCD policy, payer requirements, gender-specific regulations, and any other specialty-specific rules for your practice.