Mastering Healthcare Finances: The Role of a Medical Billing Coding Specialist
A Medical Billing Coding Specialist is a key part of the health industry, serving as a intermediary between insurance companies and healthcare providers. These professionals are accountable to translate diagnostic procedures and medical treatments and treatments into the standardized codes that are used to bill. Their work assures healthcare professionals get timely and accurate reimbursement for their services.
Importance in the Healthcare System
In a world where accuracy and precision are crucial medical billing coding specialist benefit ensure the health and financial wellbeing of hospitals. They not just assure the compliance with regulations, but also play an important part in governing revenues, which is vital to the long-term sustainability of the healthcare system.
The Role of the Medical Billing Coding Specialist
Core Responsibilities:
- Translation of Medical Records: Convert patient data to universal codes for medical care.
- Claims Submission: Send the coded documents to insurance companies to receive reimbursement.
- Reviewing the Codes: Verify that you have the most current codes and are up-to-date.
- Communicating with Providers: work with healthcare professionals in order to clarify the diagnosis or procedure.
- Management of the Patient Billing: Answer questions from patients or billing issues.
Skills Required:
- Attention to Detail: High accuracy in billing and coding.
- Experience with Medical Terminology: Learn to comprehend Medical terms as well as their meanings.
- Technical Expertise: Experience with codes and software for Electronic medical records (EHR).
- Analytical Skills: Ability to review the medical record and assure the compliance of regulations.
- Communications Skills: Effective communication with health care providers as well as insurance firms.
Education and Certification
Educational Pathways:
- Associate’s Degree in Health Information Technology: Complete training on medical billing coding specialist as well as Coding.
- Certificate Programs Shorter courses focusing on particular programming knowledge.
Certification Options:
- Certified Career-Oriented Coder (CPC): Offered by the American Academy of occupational Coders (AAPC).
- Accredited Coding Specialist (CCS) The course is offered through the American Health Information Management Association (AHIMA).
- Certified Billing and Coding Specialist (CBCS): It is provided through the National Healthcareer Association (NHA).
Different Types of Medical Codes
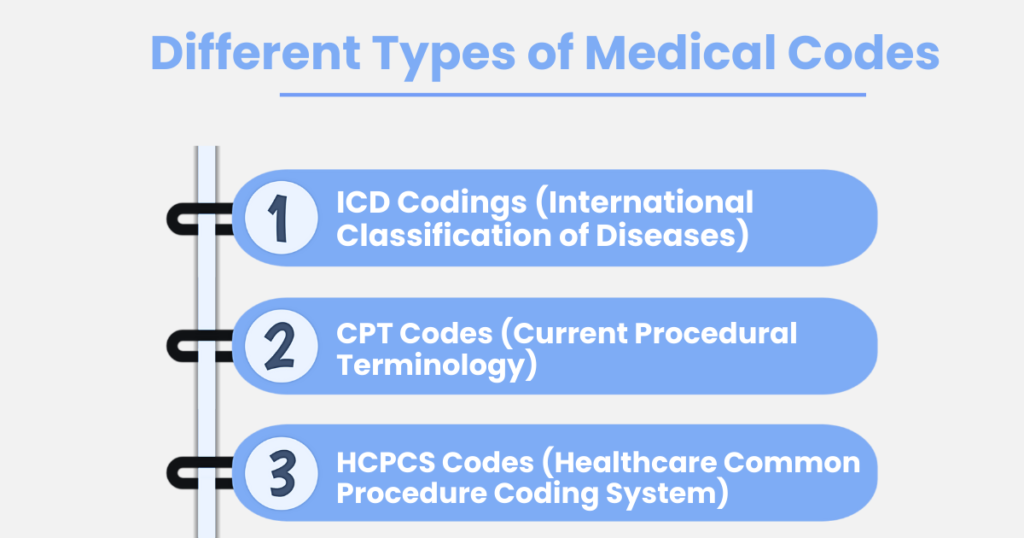
ICD Codings (International Classification of Diseases):
ICD-10-CM is a coding system primarily used for diagnosing and coding various medical conditions. It provides a detailed and standardized method for documenting diagnoses across different healthcare settings. On the other hand, ICD-10-PCS is utilized specifically for coding procedures performed during inpatient hospital stays. This system offers a comprehensive framework for accurately representing complex procedures and treatments carried out in a hospital environment, ensuring precise and consistent documentation.
CPT Codes (Current Procedural Terminology):
Category that facilitate the documentation of procedures and services. Codes are used for tracking performance and measuring quality. Codes can provide temporary solutions for new technologies and services. Together, these categories ensure comprehensive and up-to-date coding in healthcare.
HCPCS Codes (Healthcare Common Procedure Coding System):
Stage I codes are equivalent to CPT codes, used for documenting and billing various medical procedures and services provided by healthcare professionals. Stage II codes, however, focus on non-physician-related services, including ambulance services and the use of heavy medical apparatus. These codes ensure that specialized services and equipment are accurately recorded and reimbursed, reflecting their essential role in patient care.
Medical Billing Process
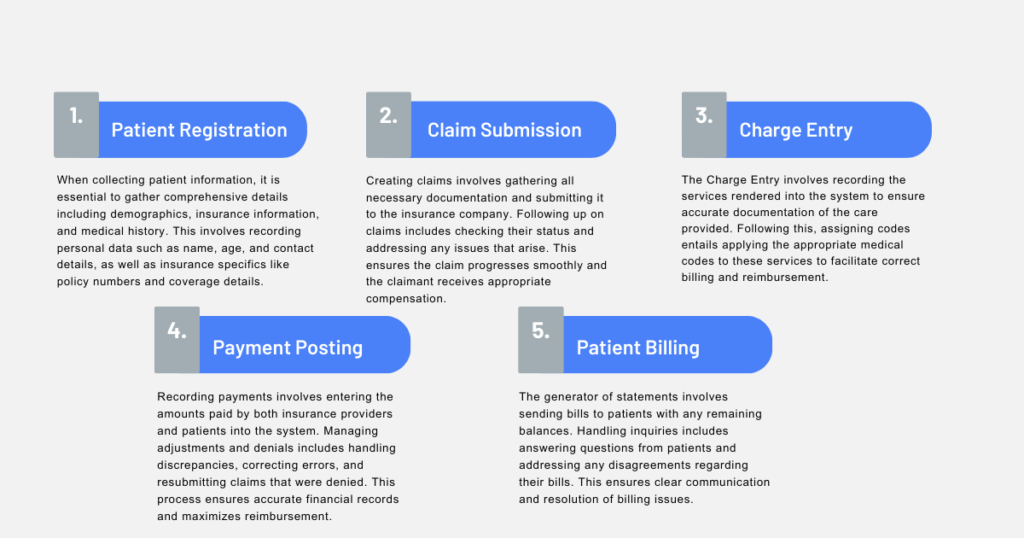
Patient Registration:
When collecting patient information, it is essential to gather comprehensive details including demographics, insurance information, and medical history. This involves recording personal data such as name, age, and contact details, as well as insurance specifics like policy numbers and coverage details. Additionally, it is crucial to verify the patient’s insurance to ensure that it covers the required services. This step involves checking the insurance policy to confirm that the patient’s coverage aligns with the medical services they are about to receive, thereby preventing any unexpected out-of-pocket expenses.
Charge Entry:
The Charge Entry involves recording the services rendered into the system to ensure accurate documentation of the care provided. Following this, assigning codes entails applying the appropriate medical codes to these services to facilitate correct billing and reimbursement. This process ensures that each service is properly categorized and billed according to established standards. Accurate entry and coding are crucial for maintaining financial and operational efficiency in healthcare settings.
Claim Submission:
Claims Submission involves gathering all necessary documentation and submitting it to the insurance company. Following up on claims includes checking their status and addressing any issues that arise. This ensures the claim progresses smoothly and the claimant receives appropriate compensation.
Payment Posting:
Recording payments involves entering the amounts paid by both insurance providers and patients into the system. Managing adjustments and denials includes handling discrepancies, correcting errors, and resubmitting claims that were denied. This process ensures accurate financial records and maximizes reimbursement.
Patient Billing:
The generator of statements involves sending bills to patients with any remaining balances. Handling inquiries includes answering questions from patients and addressing any disagreements regarding their bills. This ensures clear communication and resolution of billing issues.
Challenges in Medical Billing Coding Specialist
- Regular revisions to the coding standards and regulations requires continuous learning.
- Eliminating code errors which could result in claims being denied.
- Navigating different insurance plans and their particular needs.
- Processing rejected claims, and making sure reimbursement.
- Privacy of patient data and safety.
- Respecting the law regarding medical bills.
FAQs: Mastering Healthcare Finances: The Role of a Medical Billing Coding Specialist
What is a Medical Billing Coding Specialist?
A Medical Billing Coding Specialist is a professional who translates medical procedures and diagnoses into standardized codes for billing purposes. They act as an intermediary between healthcare providers and insurance companies to ensure accurate reimbursement for services rendered.
Why is the role of a Medical Billing Coding Specialist important in healthcare?
Medical Billing Coding Specialists ensure the accuracy and compliance of billing processes, which is vital for the financial health of healthcare facilities. Their work helps maintain revenue flow, supports regulatory compliance, and contributes to the overall efficiency of healthcare systems.
What skills are essential for a Medical Billing Coding Specialist?
Key skills include attention to detail, knowledge of medical terminology, technical expertise in coding systems and EHR software, strong analytical abilities, and effective communication skills for interacting with healthcare providers and insurance companies.
What challenges do Medical Billing Coding Specialists face?
Challenges include keeping up with regular updates to coding standards, avoiding coding errors that could lead to claim denials, navigating various insurance requirements, and ensuring patient data privacy and regulatory compliance.
What are the main coding systems used by Medical Billing Coding Specialists?
The primary coding systems include ICD-10-CM for diagnoses, ICD-10-PCS for inpatient procedures, CPT codes for documenting medical services, and HCPCS codes for non-physician services and equipment.